Conditions affecting the retina and vitreous humour
Our retina ophthalmologist specialises in treating diseases of the retina.
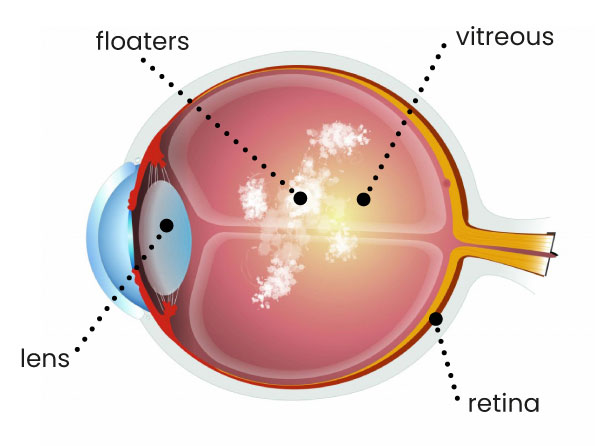
Floaters
What are floaters?
If you see black, floating spots, dots or lines in your field of vision, especially against a light background like a computer screen or bright light, that may mean you have ‘floaters’.
These spots move slowly with the movement of your eyes and always look like they are returning to their starting position. They can occur in one eye or both eyes. Floaters are structures that move around in the vitreous, the gel that fills your eyes. Although these are mostly harmless and just a bit annoying, floaters are sometimes a symptom of another condition. Follow-up by your eye doctor is therefore required.
- Black, floating spots, dots or lines in the field of vision
- Noticeable against light backgrounds, such as a computer screen, white surface or clear sky
- Spots that move with your eyeball in the direction you are lookin
- In one eye or both eyes

During a preliminary examination, your eye doctor will look into your eye to assess the retina and the vitreous. To do so, the pupil is dilated as far as possible with drops. Driving afterwards is not possible for at least three hours. Sometimes the retina cannot be assessed properly. In that case, we will use an ultrasound device to see whether your retina has become detached. This examination is painless and safe.
If the cause of the floaters is a posterior vitreous detachment, then no treatment is needed or possible. The floating spots will become less annoying over time, but they usually do not disappear completely. Flashes of light generally stop on their own or if the vitreous no longer pulls away from the retina. Sometimes, floaters are an indication of an underlying eye condition that requires further treatment.
In extreme cases, the floaters need to be removed by an operation, known as a Vitrectomy, whereby the entire vitreous is removed.
Age-related macular degeneration (AMD)
What is age-related macular degeneration?
Age-related macular degeneration (AMD) is a condition of the central part of the retina. This part of the retina, the macula, is responsible for seeing small details. Age-related macular degeneration is often referred to as the ‘wearing’ of the retina or ageing of the retina. AMD affects visual acuity. This can be due to such factors as an hereditary condition, age or environmental factors.

- Less clear or fuzzy near vision
- Dark spots or dots at the centre of the image
- Difficulties in reading and in recognizing faces
- Distortion of the image, especially of straight lines
- Fading of colours
- Reduced night vision
We start with a detailed examination to determine what form of macular generation you have. This can be either dry or wet age-related macular degeneration. Each form requires a different approach, and so a correct diagnosis is crucial.
What treatments do we offer?
Injections
The principal treatment for wet AMD is anti-VEGF injections, such as ranibizumab, bevacizumab and aflibercept. These stop abnormal blood vessel growth and reduce eye leakage. After a monthly initial injection, the frequency of the follow-up injections will be determined depending on the check-up results – often four to six times a year. Although the injections are effective, they don’t guarantee complete restoration of vision; they mainly stabilise the condition. Regular check-ups by the eye doctor are essential for optimal treatment.
Photodynamic therapy (PDT)
Photodynamic therapy can be used in certain cases of wet AMD. In this process, a light-sensitive medicine known as verteporfin is injected into the bloodstream. The medicine is then activated by laser light and will attack and destroy selective abnormal blood vessels in the macula
Combination therapy
In some cases, a combination of treatments may be recommended. This can involve the simultaneous use of anti-VEGF injections and photodynamic therapy, in order to address and maximise the treatment outcomes of various aspects of the condition. Combination therapy is only applied in exceptional cases.
Laser photocoagulation
Although this is performed less often, laser photocoagulation can be considered in certain cases of wet AMD. In the past, a laser was used to close off or destroy abnormal blood vessels in the macula. Laser photocoagulation is used mostly for smaller, well-defined areas of abnormal blood vessels that are not in the central field of vision.
Sometimes a laser is used to reduce the drusen and thereby prevent further progress of wet AMD. This treatment is still a subject of discussion, however.
We start with a detailed examination to determine what form of macular generation you have. This can be either dry or wet age-related macular degeneration. Each form requires a different approach, and so a correct diagnosis is crucial to determine the correct treatment and the costs of the treatment.
Diabetic retinopathy
What is retinopathy?
If you have diabetes, the blood vessels in the retina may be affected. This is known as diabetic retinopathy. This form of damage to the retina due to leaking or abnormal blood vessels can lead to a deterioration of vision or even blindness. Regular check-ups by your eye doctor are therefore very important.
- Blurry vision
- Spots or floating spots in the field of vision
- Distortion of the image, especially of straight lines
Our eye doctors can close off leaking blood vessels with a laser treatment. The treatment takes half an hour at most. The laser treatment can slow or sometimes even stop the deterioration of vision, but it cannot heal retinopathy. Thus the decline in the quality of the retina may continue. It may be necessary for the laser treatment to be repeated several times. Diabetic patients have greater risk of tears and detachment of the retina. Small tears can be closed up with laser surgery. In the event of retinal detachment, an operation is required. This operation, known as a Vitrectomy, is performed in a hospital.
The cost of retinopathy treatment depends on your specific situation and the type of treatment chosen and will be discussed during the consultation. These treatments are covered by medical insurance.
Vitrectomy
What is vitrectomy?
Vitrectomy is an operation on the vitreous and/or retina. You may need this type of operation if you suffer from a condition of the retina or vitreous, such as in the case of floaters, diabetic retinopathy or a detached retina.
Depending on the seriousness of the condition, a vitrectomy may take between half an hour or a few hours. The operation is performed under local or general anaesthesia. In the case of vitrectomy, three small incisions are made in the white of your eye. Via these incisions, the ophthalmologist can treat your retina or vitreous problem.
If you are aged 50 or older, your ocular lens will be removed and replaced with an artificial one. We do this out of precaution, since your age increases your chance of cataracts once you have had a vitrectomy. This is discussed with you in advance.
With a vitrectomy, you are admitted to an outpatient ward in a hospital. Mostly you can go home the same day or the next day.
Around an hour before the start of the operation, you will be administered a pill under the eyelid in order to dilate your pupil. In younger patients in particular, this may still have an effect on your pupil a few days after the operation.
If you have opted for general anaesthesia, you won’t notice anything. If you opt for a local anaesthesia, you will also notice little or nothing of the operation. A vitrectomy is performed using a microscope. Looking into the bright light of the microscope can sometimes feel unpleasant. Your retina condition is then treated, as agreed, via three small incisions in the eye. At the end of the operation, your eye is filled up again with a special fluid and antibiotics are administered to protect you from a potential infection. Lastly, an eye shield will be placed over your eye(s), which you will need to keep on until the morning after the operation.
After a vitrectomy, your vision will gradually improve. This recovery may take a few weeks or months, and so you will have to be patient. You may have to use eye drops during the first weeks following the operation, in consultation with the doctor or nurse. After one or more weeks following the operation, you can resume your daily activities, but until then you will not be allowed to work.
The cost of the operation can vary, depending on the medication used and whether or not your lens had to be replaced during the operation. The costs will be discussed during the consultation. This type of operation is covered by medical insurance.